Content Warning: Discussions of Miscarriage; Grief
A fourth-year medicine student recounts the experience of working at a fertility clinic in Adelaide for his medical elective.
I arrive at 7:15am on Monday morning at the Ad elaide fertility clinic where I’m doing my medical elective placement to observe the first surgery of
the day.
In the theatre, I scan the list of times, doctors, and notes, and my eyes alight on an unfamiliar acronym under ‘Procedure’ for the last case: ERPC.
With a sudden sadness I unravel the meaning in my mind: Evacuation of Retained Products of Conception.
In the general population, some women are not even aware that they are pregnant when fetal demise occurs very early in pregnancy. For others, there is no way to know if fetal demise has occurred in the absence of fetal movements in the first trimester, and the miscarriage ensues naturally. For women pregnant through IVF and other assisted reproductive technologies however, frequent monitoring means early detection of fetal demise and the option of removing the conceptus surgically.
On a practical level, this means that a woman can begin another treatment cycle sooner, and potentially give herself the best chance of a successful pregnancy in the face of a ticking biological clock. On another, and according to my supervisor, once women have learned of the demise of their baby, most prefer to have it removed. The idea of your baby being essentially dead inside you and having to wait for it to pass unpredictably in the days or weeks ahead is understandably unappealing.
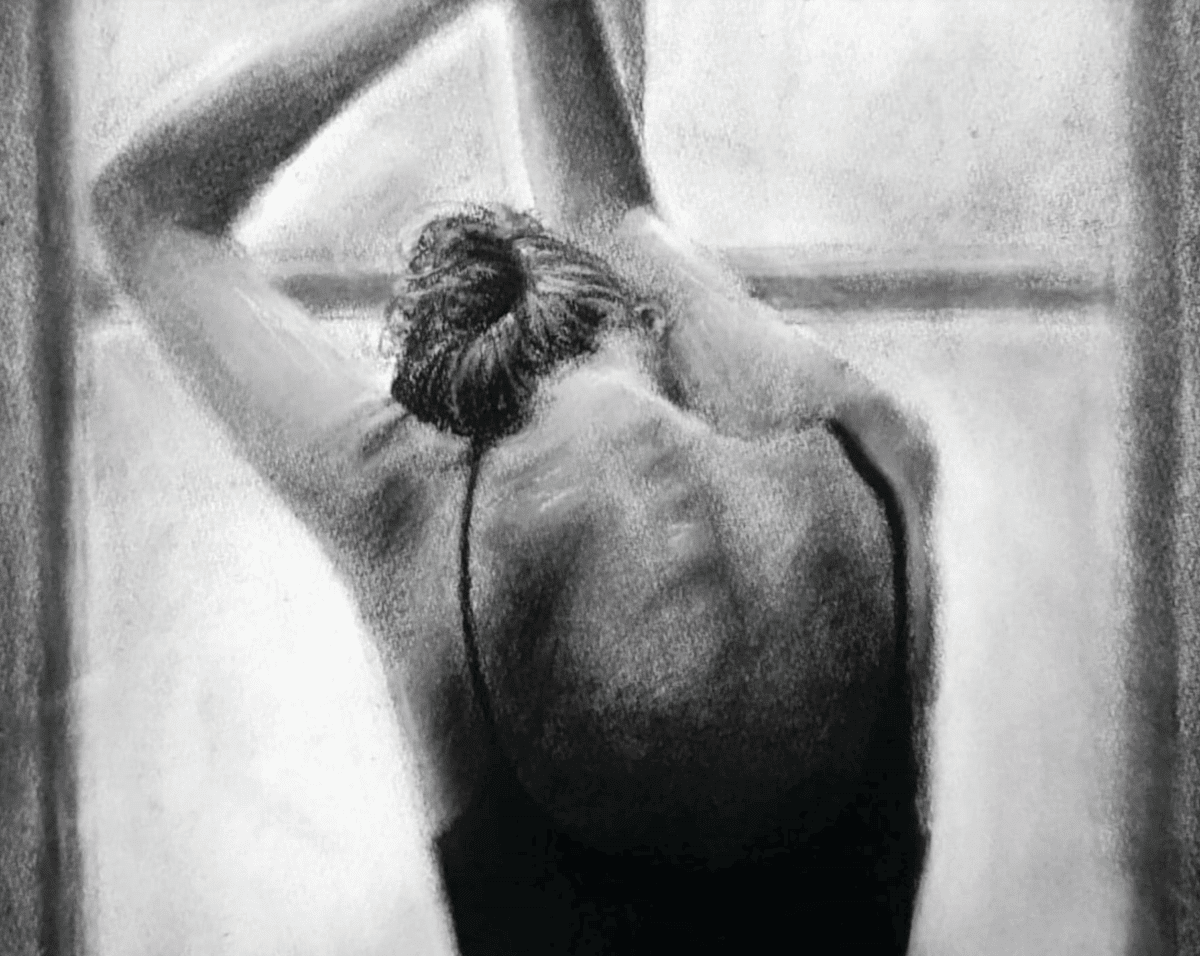
Around 12:30pm, after a dozen or so routine oocyte collections, the ERPC patient is brought into the theatre by the anaesthetic nurse and introduced to the surgical team. She appears wrung out and tired, and is taking small steps like an elderly Parkinson’s patient, although she is young.
She struggles to meet any eyes in the room.
My supervisor introduces herself and expresses her sympathy – the patient looks up briefly and they share a momentary connection. She has had some bleeding this morning, so my supervisor explains that she will need to perform a scan to determine what, if anything, remains in situ.
The patient is lain upon the surgical table and the procedure commences. I see the patient wince slightly as the ultrasound probe is introduced.
As she studies the ceiling, a single tear leaves her lateral canthus and streaks her left cheek. The radio is on, and in the quiet of the theatre, a new song starts: ‘7 days’ by Craig David.
As I watch the patient I suspect that this experience is searing into her memory. She seems to be listening to the music, possibly to distract herself, and I wonder if she’ll ever hear this song again without thinking of this moment.
The chorus swells:
“…I met this girl on Monday
Took her for a drink on Tuesday
We were making love by Wednesday
And on Thursday and Friday and Saturday
We chilled on Sunday”
And it strikes me how much life has changed for this patient over the course of the last seven days, and how volatile the healthcare journey can be for patients dealing with infertility:
Blissfully pregnant on Monday
Had some spotting on Tuesday
No fetal heart seen on Wednesday
And on Thursday and Friday and Saturday
We cried on Sunday
The uterus contains fetal material, and the patient is put under sedation for the ERPC.
Afterwards, as I help the nurses clean the theatre, specimens are prepared for histology and karotyping, and I watch as she is wheeled into recovery.
I hope that the next seven days are a little easier for her than the last.
We acknowledge the Ngunnawal and Ngambri people, who are the Traditional Custodians of the land on which Woroni, Woroni Radio and Woroni TV are created, edited, published, printed and distributed. We pay our respects to Elders past and present. We acknowledge that the name Woroni was taken from the Wadi Wadi Nation without permission, and we are striving to do better for future reconciliation.